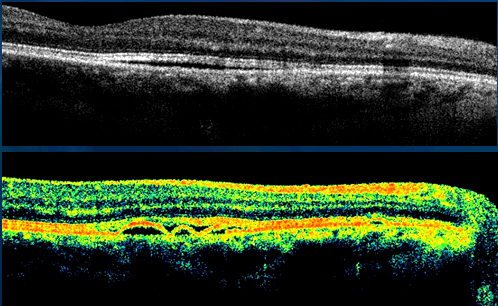
Optical Coherence Tomography (OCT)
 This is the latest & first imaging technique that provides minutest information (upto 10 microns) regarding the retinal layers using laser technology. OCT is most commonly used to diagnose macular disorders like macular hole, macular pucker, and diabetic retinopathy. OCT is a non-invasive technology used for imaging the retina, the multi-layered sensory tissue lining the back of the eye. OCT, the first instrument to allow doctors to see cross-sectional images of the retina, is revolutionizing the early detection and treatment of eye conditions such as macular holes, pre-retinal membranes, macular swelling and even optic nerve.
This is the latest & first imaging technique that provides minutest information (upto 10 microns) regarding the retinal layers using laser technology. OCT is most commonly used to diagnose macular disorders like macular hole, macular pucker, and diabetic retinopathy. OCT is a non-invasive technology used for imaging the retina, the multi-layered sensory tissue lining the back of the eye. OCT, the first instrument to allow doctors to see cross-sectional images of the retina, is revolutionizing the early detection and treatment of eye conditions such as macular holes, pre-retinal membranes, macular swelling and even optic nerve.
Similar to CT scans of internal organs, OCT uses the optical backscattering of light to rapidly scan the eye and describe a pixel representation of the anatomic layers within the retina. Each of these ten important layers can be differentiated and their thickness can be measured. , OCT uses the optical backscattering of light to rapidly scan the eye and describe a pixel representation of the anatomic layers within the retina. Each of these ten important layers can be differentiated and their thickness can be measured. Clinic, in Ohio.
For certain conditions, such as age-related macular degeneration and cystoid macular edema, the 45 second OCT procedure is able to reduce or even eliminate the need for fluorescein angiography for some patients
![]() Click here to see presentation Optical Coherence Tomography procedures at Apollo Eye Hospitals – By Dr. Mallika Goyal
Click here to see presentation Optical Coherence Tomography procedures at Apollo Eye Hospitals – By Dr. Mallika Goyal
![]()
Retinal Angiography ( Fundus Fluorescein Angiography)
It proves to be a great help in diagnosis and treatment of a variety of retinal conditions by demonstrating various features which are not visible on clinical examination. It also documents the retinal conditions for future progress.
Fluorescein Angiography
 Fluorescein angiography, a clinical test to look at blood circulation inside the back of the eye, aids in the diagnosis of retinal conditions associated with diabetes, age-related macular degeneration, and other eye abnormalities. The test can also help monitor the course of a disease and its treatment. It may be repeated on multiple occasions.
Fluorescein angiography, a clinical test to look at blood circulation inside the back of the eye, aids in the diagnosis of retinal conditions associated with diabetes, age-related macular degeneration, and other eye abnormalities. The test can also help monitor the course of a disease and its treatment. It may be repeated on multiple occasions.
Fluorescein, an orange-red dye, is injected into a vein in the arm. The dye travels through the body to the blood vessels in the retina. A special camera with a filter flashes a blue light into the eye and takes multiple photographs of the retina. No X-rays are involved.
If there are abnormal blood vessels, the dye leaks into the retina or stains the blood vessels. Damage to the lining of the retina or atypical new blood vessels may be revealed as well. These abnormalities are determined through a careful interpretation of the photographs by an ophthalmologist.
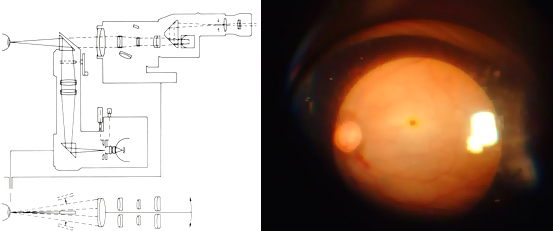
The dye can discolor skin and urine until it is removed from the body by the kidneys. There is little risk in having fluorescein angiography, though some people may have mild allergic reactions to the dye. Severe allergic reactions do occur.. Being allergic to X-ray dyes with iodine does not mean you’ll be allergic to fluorescein. Occasionally, some of the dye leaks out of the vein at the injection site, causing a slight burning sensation because of the salt that is in the dye.
![]() Click here to see presentation on Fundus Fluorescein Angiography procedures at Apollo Eye Hospitals – By Dr. Mallika Goyal
Click here to see presentation on Fundus Fluorescein Angiography procedures at Apollo Eye Hospitals – By Dr. Mallika Goyal
![]()
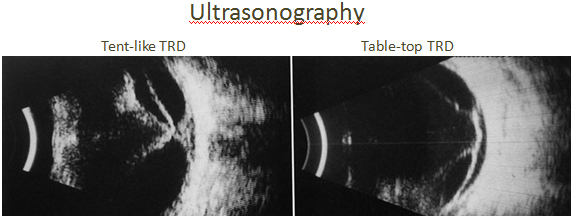
Ultrasonography (B-SCAN)
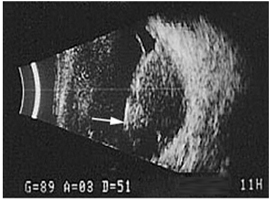 This is a simple non-invasive test that uses sound wavesto see the internal eye structures. It is a test performed when the inner parts of the eye are not visible due to opacities such as a dense cataract, vitreous hemorrhage. Ophthalmic ultrasonography uses high-frequency sound waves, which are transmitted from a probe into the eye. As the sound waves strike intraocular structures, they are reflected back to the probe and converted into an electric signal. The signal is subsequently reconstructed as an image on a monitor, which can be used to make a dynamic evaluation of the eye or can be photographed to document pathology. The image is reconstructed by the computer and the printout gives a fair idea of the status of the ocular structures like retina. This test helps in diagnosis and planning the management. It also helps us in predicting the outcome of the treatment.
This is a simple non-invasive test that uses sound wavesto see the internal eye structures. It is a test performed when the inner parts of the eye are not visible due to opacities such as a dense cataract, vitreous hemorrhage. Ophthalmic ultrasonography uses high-frequency sound waves, which are transmitted from a probe into the eye. As the sound waves strike intraocular structures, they are reflected back to the probe and converted into an electric signal. The signal is subsequently reconstructed as an image on a monitor, which can be used to make a dynamic evaluation of the eye or can be photographed to document pathology. The image is reconstructed by the computer and the printout gives a fair idea of the status of the ocular structures like retina. This test helps in diagnosis and planning the management. It also helps us in predicting the outcome of the treatment.
B-scan ultrasonography is most useful when direct visualization of intraocular structures is difficult or impossible. It tells us about the state of the vitreous. The ultrasound can detect retinal detachment, traction on the retina, retinal tears and tumors. It can be used to study the choroid to look for choroidal thickening, choroidal detachment and masses and the optic nerve for swelling or gross glaucomatous cupping.
![]()
Indirect Ophthalmoscopy
This is a special OPD procedure for examining the retina using a head mounted instrument. This method is the best way of seeing the retinal periphery for any holes, tears & Retinal Detachment. It is used extensively in retinal detachment surgery and is also the only way to see the retina through a significant cataract or vitreous haze. Advantage of this method over the others is that a magnified view of a large part of the retina can be seen.
It is essential to dilate the pupils for this test. The dilating drops are put into the eye and this takes about 30 minutes. Because of this dilatation, there is increased glare, especially in the sun. The near objects appear hazy for approximately 4-6 hours. We recommend you should not drive after dilatation and should have someone else to drive you back home.
![]()
Amsler Grid
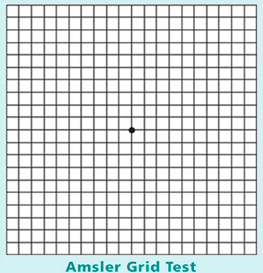 One way to test the central vision in order to detect even the smallest changes when they first appear is to use the Amsler grid.
One way to test the central vision in order to detect even the smallest changes when they first appear is to use the Amsler grid.
The Amsler grid is not the only way to watch for symptoms of macular degeneration. You can also check your vision using a book or newspaper. Many people find that a crossword puzzle or Venetian blinds work as well as the Amsler grid to reveal distortion. Digital clocks are useful in exposing blank areas in the central vision. The key is to look at the same object from the same distance in the same way (with or without glasses) using only one eye at a time, each time you check your vision. If you think there is a change, but you aren’t sure, it is safe to wait a day or two and check your vision again. If it is anything to worry about, the disturbance in your vision will not go away – if anything, it may get worse.
![]()
Perimetry
Perimetry is a visual field test of the eye that checks for problems of peripheral (side) vision. Peripheral vision is used primarily for detecting objects and for directing central vision so it is possible to see those objects in detail. A loss of peripheral vision results in a condition called tunnel vision and can lead to blindness.
When is a perimetry test administered?
The cells that make up the retina are responsible for the ability to see detail, brightness, and color. There are two types of photoreceptor cells in the cornea — rods and cones. The rods specialize in work at low light levels, and the cones provide sharp vision, color, and contrast discrimination. People with achromatopsia have defective cone cells and must rely on their rod photoreceptors for vision.
In normal eyes, there are about 6 million cone photoreceptors, located mainly in the macula at the center of the retina (See Anatomy of the Eye). These cells are primarily responsible for sharp, straight-ahead vision and also for the ability to distinguish colors. There are 100 million rod receptors, located mostly at the periphery of the retina. The rods are more sensitive to light than cones are, but rods are not able to differentiate among colors, nor can they perceive shades of gray, black, and white.
There are different variations in the severity of symptoms among individuals with achromatopsia. The rarest and most severe is called complete rod monochromatism, where there is a total lack of cone function. People with this disorder are extremely sensitive to light, even in normally lit rooms. They also have symptoms of poor visual acuity and nystagmus, which is involuntary movement of the eyes. Other less severe variations of the disorder are known as incomplete rod monochromatism and blue cone monochromatism. The type depends on which cones are affected.
How is a perimetry test conducted?
A perimetry test is easy and comfortable. Sometimes a doctor administers the test, but usually a trained technician administers it. To take the test, you sit with your head in a chin rest at the edge of a large, bowl-shaped instrument with a fixed spot in the center — usually a yellow or green light.
There are two types of perimetry tests. In the Goldman kinetic perimeter test, you stare directly at the spot as the technician moves objects or lights of different size and brightness from the side. When you see the object or light, you push a button.
The threshold static automated perimetry, which is the other type of perimeter test, uses stationary objects of light that blink on and off in various parts of the visual field.
With either method, each eye is tested independently. The maps of visual sensitivity, made by either of these methods, are very important in diagnosing diseases of the visual system.
The perimetry test usually takes no more than 30 minutes, and the results are available immediately.
![]()
