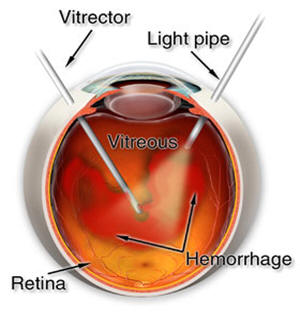
Vitrectomy is a microsurgical procedure in which specialized instruments and techniques are used to repair retinal disorders, many of which were previously considered inoperable. The initial step in this procedure is usually the removal of the vitreous gel through very small (~1.4mm) incisions in the eye wall, hence the name “vitrectomy”. The vitreous is removed with a miniature handheld cutting device and replaced with a special saline solution similar to the liquid being removed from the eye. A high intensity fiberoptic light source is used to illuminate the inside of the eye while the surgeon works. The surgeon uses a specialized operating microscope and contact lenses, which allow a clear view of the vitreous cavity and retina at various magnifications. The procedure is performed in an operating room under local or (occasionally) general anesthesia. It can often be done as an ambulatory procedure.
Although vitrectomy procedures are sometimes performed through incisions made near the front of the eye, most vitreoretinal surgeons enter the globe through a part of the eye known as the pars plana. This is why the procedure is often referred to as a trans pars plana vitrectomy (TPPV). Entering the eye through this location avoids damage to the retina and the crystalline lens.
Pars plana vitrectomy is used to treat many different retinal disorders including those listed below (more information on some of these topics can be found elsewhere in our patient information section):
1. Proliferative diabetic retinopathy (including vitreous hemorrhage)
2. Macular hole
3. Macular pucker (Epiretinal membrane)
4. Complicated, tractional or recurrent or retinal detachment
5. Intraocular infections (endophthalmitis)
6. Intraocular foreign body
7. Retained lens material or dislocated lens implants following cataract surgery
8. Giant retinal tears
9. Traumatic eye injuries
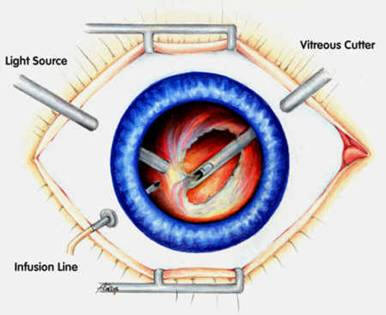
Surgeon’s view during vitrectomy surgery
During vitrectomy surgery, the retinal surgeon may use a variety of special techniques to achieve the desired results, including:
![]() Intraocular gases (usuallyeither perfluropropane (C3F8) or sulfur hexafluoride (SF6)) when mixed with sterile air have the property of remaining in the eye for extended periods of time (up to two months). They are eventually replaced by the eyes own natural fluid. Gas is useful for flattening a detached retina and keeping it attached while healing occurs. Gas injection is also used to close macular holes. It is frequently necessary to maintain a certain head position following surgery when gas is used. Vision in a gas filled eye is usually rather poor until at least 50% of the gas is absorbed. Possible complications of intraocular gas include progression of cataracts and elevated eye pressure (glaucoma). It is unsafe to fly in a plane while gas remains in the eye.
Intraocular gases (usuallyeither perfluropropane (C3F8) or sulfur hexafluoride (SF6)) when mixed with sterile air have the property of remaining in the eye for extended periods of time (up to two months). They are eventually replaced by the eyes own natural fluid. Gas is useful for flattening a detached retina and keeping it attached while healing occurs. Gas injection is also used to close macular holes. It is frequently necessary to maintain a certain head position following surgery when gas is used. Vision in a gas filled eye is usually rather poor until at least 50% of the gas is absorbed. Possible complications of intraocular gas include progression of cataracts and elevated eye pressure (glaucoma). It is unsafe to fly in a plane while gas remains in the eye.
![]() Silicone oil is sometimes used instead of gas to keep the retina attached postoperatively. Silicone remains in the eye until it is removed (often necessitating a second surgery at a later date). This technique is advantageous when long term support (“tamponade”) of the retina is required, for instance in the repair of very complicated retinal detachments. Unlike gas, patients are still able to see through clear silicone oil. Positioning is less critical with silicone oil, therefore, it may be used in patients unable to position postoperatively (i.e. children). Like gas, silicone oil can promote cataracts, cause glaucoma, and may damage the cornea.
Silicone oil is sometimes used instead of gas to keep the retina attached postoperatively. Silicone remains in the eye until it is removed (often necessitating a second surgery at a later date). This technique is advantageous when long term support (“tamponade”) of the retina is required, for instance in the repair of very complicated retinal detachments. Unlike gas, patients are still able to see through clear silicone oil. Positioning is less critical with silicone oil, therefore, it may be used in patients unable to position postoperatively (i.e. children). Like gas, silicone oil can promote cataracts, cause glaucoma, and may damage the cornea.
![]() Endophotocoagulation is the use of laser to treat intraocular structures. This modality is often used to treat retina tears in the setting of retinal detachment. Endophotocoagulation is frequently used to treat proliferative diabetic retinopthy as well.
Endophotocoagulation is the use of laser to treat intraocular structures. This modality is often used to treat retina tears in the setting of retinal detachment. Endophotocoagulation is frequently used to treat proliferative diabetic retinopthy as well.
![]() Microsurgical instruments such as forceps, scissors and picks may be used to manipulate intraocular structures such as in the removal of scar tissue and foreign bodies. Literally hundreds of vitrectomy instruments are available to assist in different surgical maneuvers. Most of these vitreoretinal tools have a diameter of less than 1mm, making them some of the most precise and finely crafted instruments in the world today.
Microsurgical instruments such as forceps, scissors and picks may be used to manipulate intraocular structures such as in the removal of scar tissue and foreign bodies. Literally hundreds of vitrectomy instruments are available to assist in different surgical maneuvers. Most of these vitreoretinal tools have a diameter of less than 1mm, making them some of the most precise and finely crafted instruments in the world today.
![]() Endoscopy allows the surgeon to view the inside of the eye on a television monitor while treating intraocular structures. It is a helpful technique when the cornea or lens are cloudy and do not allow a clear view through the operating microscope.
Endoscopy allows the surgeon to view the inside of the eye on a television monitor while treating intraocular structures. It is a helpful technique when the cornea or lens are cloudy and do not allow a clear view through the operating microscope.
![]() Scleral buckling is sometimes combined with a vitrectomy procedure to add additional support to the re-attached retina
Scleral buckling is sometimes combined with a vitrectomy procedure to add additional support to the re-attached retina
![]() Lensectomy is the removal of the eye’s crystalline lens during a vitrectomy procedure. This is sometimes performed when there is a cataract (clouding of the lens) which prevents the surgeon from adequately visualizing the internal structures. A lensectomy may also be necessary to gain access to and remove scar tissue during complicated retinal detachment or diabetic retinopathy procedures. The natural lens can be replaced with a clear lens implant at a later date or during the same surgical procedure. Lensectomy is usually performed using high frequency ultrasound (phacoemulsification) similar to routine cataract surgery.
Lensectomy is the removal of the eye’s crystalline lens during a vitrectomy procedure. This is sometimes performed when there is a cataract (clouding of the lens) which prevents the surgeon from adequately visualizing the internal structures. A lensectomy may also be necessary to gain access to and remove scar tissue during complicated retinal detachment or diabetic retinopathy procedures. The natural lens can be replaced with a clear lens implant at a later date or during the same surgical procedure. Lensectomy is usually performed using high frequency ultrasound (phacoemulsification) similar to routine cataract surgery.
Vitrectomy surgery is a major medical advance which allows us to treat retinal diseases and prevent vision loss for patients who, in previous years, may have gone blind without this technique. A vitrectomy procedure usually takes about 1-2 hours but may take longer in complex cases or when combined with a scleral buckle or lensectomy.
![]()
